As a person belonging to the so called frail population because of age over 65 and with comorbidities (hypertension and overweight), I underwent triple vaccination with the mRNA-Pfizer-Biontech vaccine (the third dose was administered on 10.11.2021).I could fly and also move around by train (always using a face mask).
It was understandable that a fourth vaccination at the beginning of the spring and of the summer would not make very much sense.However although the offically number of recorded infections was decreasing,everybody knew somebody in the own family and in the „enviroment“,who was affected by the infection although fully vaccinated. Less attention was payed
to wearing face masks especially in crowded interiors such as restaurants.
Three days after a nice dinner with some wine(saturday 11.06.2022),which lasted about three hours with friends a mild but fastidious headhache began to occupy my imagination. I tried to understand the cause.I was feeling a vey mild sore throat when my friend called me to tell me that he was running a fever and that he was found to be SARS-CoV-2-positive.His wife was at first negative with no symptoms.She became later positive and had mild running nose only.
He asked me for therapeutic suggestions although he had alreasdy consulted several doctors. It was strange,“if you have fever you have to take antibiotics“ he was advised.
He also got prescribed vitamin D,C an B and nimesulide (Aulin) as an antiinflammatory drug.
I explained to him that there is no reason to take antibiotics and suggested abundant fluid intake.While discussing with ihm, I realized that I also was developing the full blown picture of a flu.In fact, my nose became closed by increasing intranasal pressure and my headhache became stronger.I started to take aspirin pills (500 mg/each) and to lay down and rested.Always accompained by a 1.5 liter bottle of water.
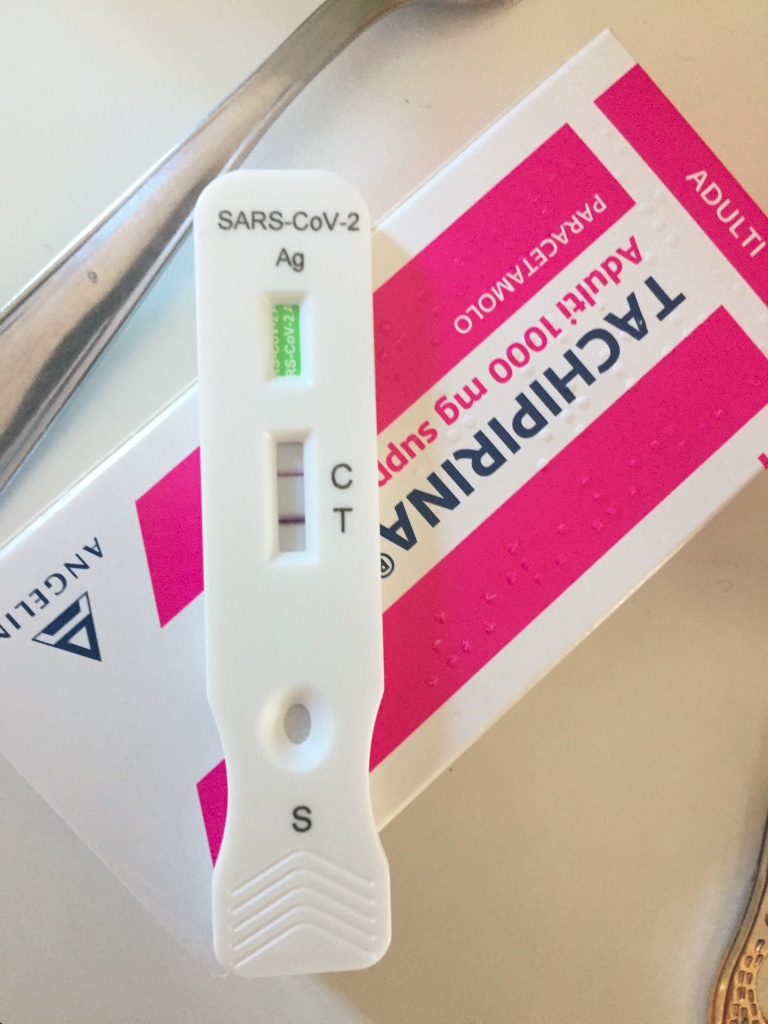
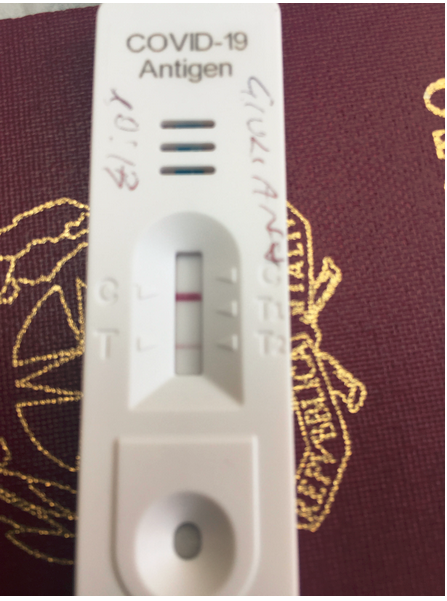
The SARS-CoV-2 Antigen Rapid Test was clearly positive, while my wife´s was negative.Body temperature was around 37 degree Centigrade.I continued to eat and drink abundantely.
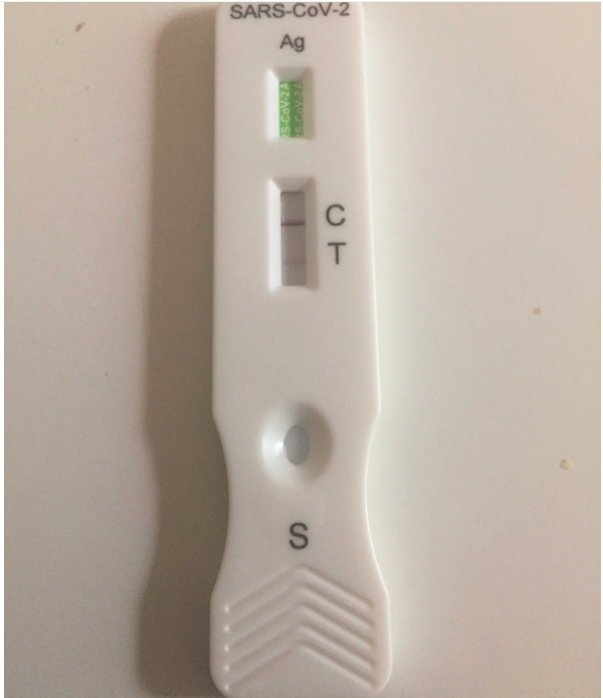
After two days of taking 2gr Aspirin/each, symptoms improved substancially and I stopped to take aspirin on the third day.Symptoms continued to improve on the third day (wihtout Aspirin).On the day 4 in absence of symptoms the rapid antigen test showed a significant decrease of the viral antigen in the nose.My wife`s test continued to be negative.I decided to continue to stay home and to perform a PCR-analysis on next monday.
SARS-CoV-2 Antigen rapid test shows a significant reduction of the viral antigen on the second day of recovery from the flu-like symptoms
PCR-analysis of the nasal RNA was positive on the 21.06.22 wit a CT-value of 33 (JAMA Intern Med. Published online April 29, 2022. doi:10.1001/jamainternmed.2022.1827).
At the same day IgM anti-spike were not detectable while IgG -antibodies against the RBD of the spike protein were measurable (620,4 Binding Antibodies Unit/ml serum 6Vol:.(1234567890)Scientific Reports | (2022) 12:8679 | https://doi.org/10.1038/s41598-022-1275).
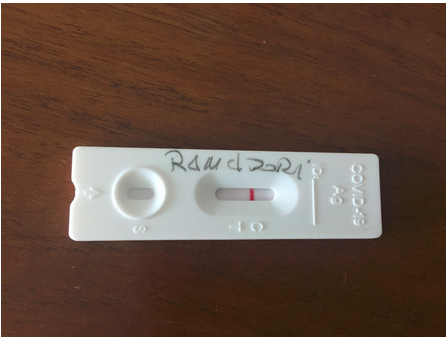
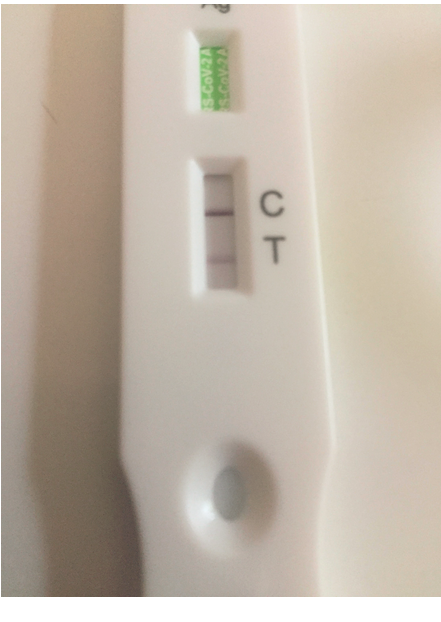
and definitively negative (LUNGENE) on saturday 25.06.22
Montegiorgio (FM),Italy ,saturday ,June 25th
Summary:
1.Infection with SARS-CoV-2 has happened in a 70 -year-old person with comorbidities 8 mounths after the third mRNA-vaccination (Pfizer/Biontech).
2.Flu-like symptoms (headasche,runny nose and mild jount pain) occurred on the third day after infection
3.one day after beginning of the symptoms rapid antigen test was clearly positive
4.immediate beginn of anti-inflammatory therapy with aspirin , 2 grams/day.
5.After two day of therapy accompanied by aboundant drinking (>3 L /day)
symptms had disappeared.
6.Antigen rapid test was still positive as it was the PCR-RNA-test (CT=33)
7.Immunoglobulin M antibodies were not detectable before 10 day after infection and
8 days after apparence of first symptoms.
8.Antigen rapid test was negative 14 days after infection and 11 days after symptoms started.
QUESTIONS:
1.if the first action to take is immediate reduction of symptoms (especially fever,headhasche,joint-pain) may just aspirin be the first choice drug in consideration of the low diffusion and accessibility of antiviral drugs(ANNALS OF MEDICINE 2022, VOL. 54, NO. 1, 516–523
https://doi.org/10.1080/07853890.2022.2034936) ?
2.why does it take so long for IgM to become detectable after 3 vaccinations?
3.were the IgG-antibodies pre-existent before infection?
4.do I need a forth vaccination or does it make sense at all? (see recent publication in JAMA JAMA Intern Med. Published online June 23, 2022. doi:10.1001/jamainternmed.2022.2658 )